The pioneering bits of medical code that will shape digital health's future
How we incorporate ethical codes into medical AI/ML algorithms will have long-term repercussions. The history of tech in medicine can give us a guide.
Medicine, philosophy, and ethics have been bound from the moment of their conception. From Confucius to Socrates, philosophers of yore infused heady existential concepts into ethical frameworks for how doctors (or healers, in earlier times) should interact with their patients and colleagues, promoting ideals of personhood, non-malfeasance, and shared knowledge to promote wider prosperity. Many of these concepts are etched into the Hippocratic oath that (ostensibly, in some form) is honored by healthcare professionals to this day.
But ethics, like science and medicine, evolve with new discovery—and that evolution raises fundamental questions about how new data, new technologies, and ensuing shifts in medical practice can be best deployed to benefit patients and society. Hippocrates himself hasn’t escaped the red pen of history as more patient-centric approaches to healthcare, including ethical standards of informed consent in the clinic, supplanted his more paternalistic ancient Greek view of the doctor-patient relationship. And that was long before AI and machine learning entered the arena.
“Contrary to popular belief, the Hippocratic Oath is not required by most modern medical schools, although some have adopted modern versions that suit many in the profession in the 21st century. It also does not explicitly contain the phrase, “First, do no harm,” which is commonly attributed to it.” - National Library of Medicine
Medical and life sciences technology is at an inflection point where its progress is tucked into algorithmic designs that can suss through a mountain of biological data, or map out the best hospital bed triage strategies, or even generate hypothetical protein structures that might spur new drugs.
“Do no harm” might not easily translate to modern algorithmic code; nonetheless, it remains a fundamental coda to which medical practitioners aspire, a human-focused end for what often boils down to programmatic steps in a treatment algorithm (i.e., what a clinician does by design at each step of a patient’s journey through their disease). It’s a delicate dance between moral obligations to public health, thorny ethical guidelines for medical workers, research scientists, and technologists alike, and the imperative to speed up successful drug development and efficient care delivery with the use of new technologies.
Choreographing that evolving dance isn’t a new enterprise. For centuries, the medical community has had to balance how to best turn data uncovered by new research into actionable intelligence—while hewing to patient-centricity standards, informed consent, non-harm, and the long-term advancement of science and broader public health without losing sight of patients’ immediate needs.
The late Martin Lipkin, a pioneering oncologist and professor at Weill Cornell Medical College in New York, latched on to the promise of computers in medicine in the 70s and 80s, spearheading revolutionary approaches for disease detection by identifying biomarkers correlated with high cancer risk (and potential targets for new medicines) based on real-world patient data.
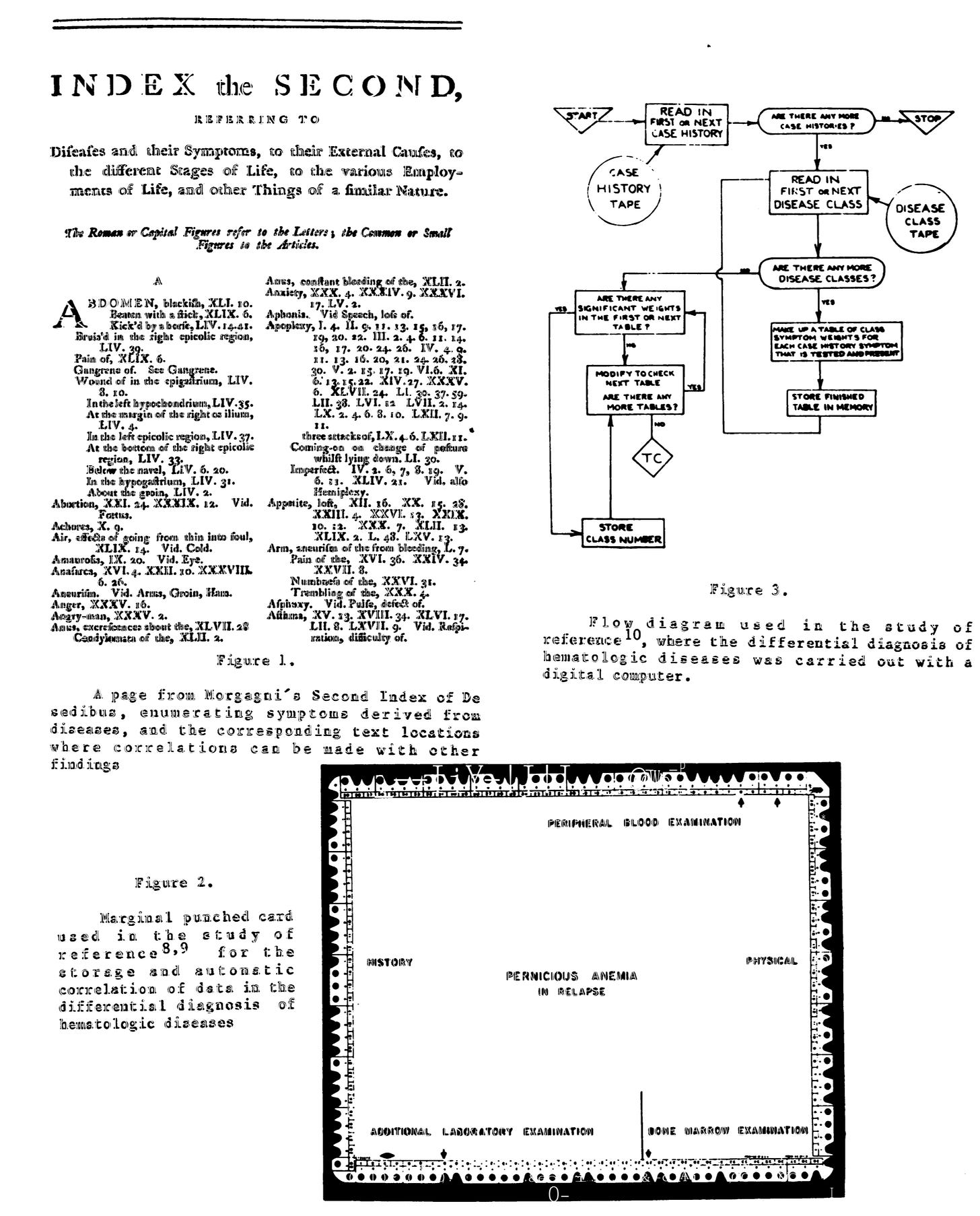
He marveled at how quickly this method—taking vast amounts of data and blending it with new tech that could crunch and correlate all of it—produced valuable insights in a 1984 journal article, likening it to a hyperspeed version of how 1950s-era computer punch cards streamlined blood disorder diagnoses based on hematological insights originally made by the 18th century anatomist Giovanni Morgagni in the 1760s.
“In 1952 punched cards were used to automatically correlate data in the differential diagnosis of hematologic diseases, and in 1961 a computer was introduced into medicine for that purpose. The many great advances in the application of computer technology that followed, in so many areas of medical research and practice, have led to revolutionary improvements in bibliographic, laboratory, radiologic and other branches of medicine, and have fulfilled expectations of those active in the field that were only hoped for several decades ago.” - Historical Background on the Origin of Medicine
The rate of technological progress and impact—alongside intertwined ethical considerations—in medicine accelerated in the decade after Lipkin’s article was published. In 1991, the national Institute of Medicine under the National Academy of Sciences released a landmark report commissioned by the federal government dubbed, “The Computer-Based Patient Record: An Essential Technology for Health Care.”
It was, as you might suspect, a report on emerging computer technologies that took paper-based patient health records to a digital format. As blasé as that might sound to the modern, Airpod-stuffed ear, the advent of the electronic medical record is a bedrock of modern digital health to the extent that it’s hard to imagine the medical advances of the past 30 years without them. And we live in an era when lines of code are used to examine entire hospitals in real-time and generate patient triage strategies to efficiently get them to available hospital beds.
Even in 1991, federal public health researchers balanced the promise of EMRs with the greater ethical obligations of setting up systems with the North Star goal of advancing ethical imperatives in medicine—the maximum good for the most number of people, the pursuit and distribution of knowledge, and insights that balance empirical efficiency with the needs of real human beings. In fact, the report begins by noting that “simple automation” made possible by electronic records should be considered a tool that serves a much larger, distal goal that balances patients’ dignity alongside society’s medical needs:
“We are not suggesting a simple automation of the current patient record. Rather, we envision the next generation of CPRs [Computer-based patient records] and CPR systems as essential to the full maturation of the scientific basis of health care. The report outlines the basic components of future CPRs and a strategic plan for achieving widespread CPR implementation. Further, it identifies the key organizations that will need to play major roles if the plan is to succeed.
The vision of the patient record of the future that emerged from the committee's deliberations seems uniquely appropriate for a nation that values pluralism and privacy and has a mobile population with growing levels of chronic illness.” - The Computer-Based Patient Record: An Essential Technology for Health Care
What will these foundational documents look like for AI and ML? How would it address long-standing disparities in medicine across race, class, and geographic location? How might it address the potential tradeoffs between patient privacy (say, in the case of biometric data collected through a range of wearable devices that might then be used for research) and the needs of society to create new medicines, or make hospitals more efficient without sacrificing care quality? Bear in mind, these are questions that also go to the heart of science—the very data fed into new machines, which is imperfect and incomplete.
These are some of the key, complex questions that industry and government are actively parsing today following President Joe Biden’s executive order on AI in American industry—an order which largely centers on AI/ML’s use in healthcare and drug development.
It’s an issue I’d also love to hear readers’ thoughts about—this is, after all, the central theme for Phase 5. Feel free to shoot me a note, even if it’s just a passing thought.
For now, here’s one conceptual framework balancing the medical ethics developed by the likes of Hippocrates, Thomas Percival (the 19th century British doctor who might have coined the term “medical ethics” in the first place), and so many others.
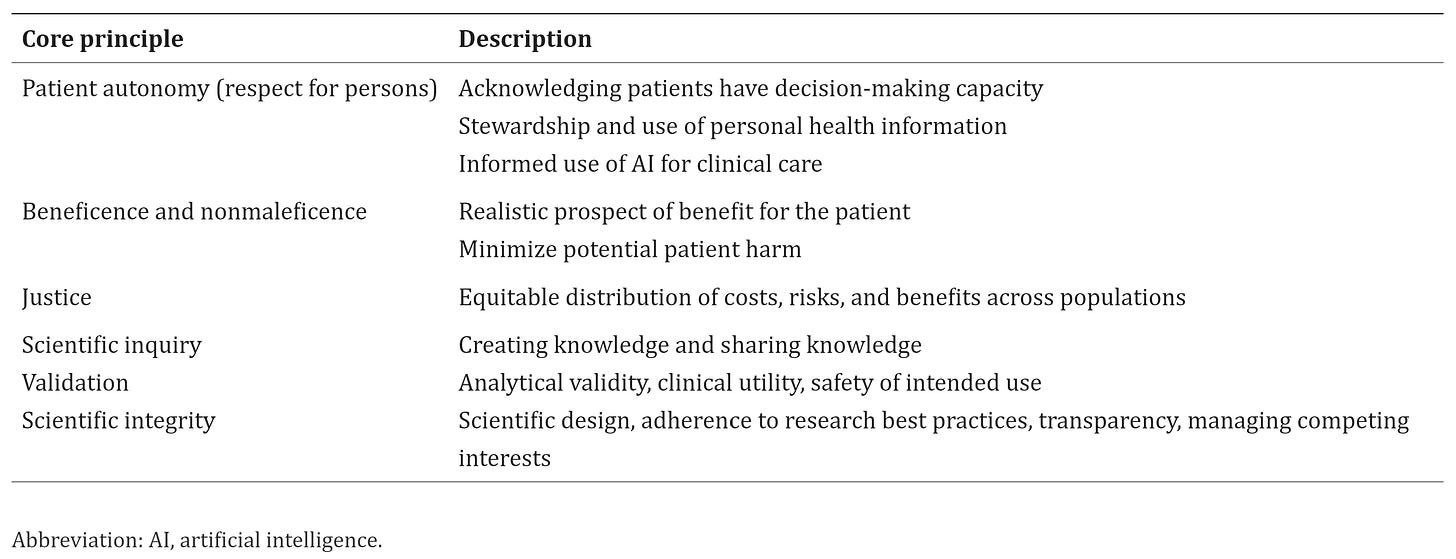
This is a specific use case for the role AI/ML might play in pathology and laboratory medicine from a 2021 journal article written by a federation of doctors and medical researchers spanning the University of Utah School of Medicine, Cincinnati Children’s Hospital, the University of Michigan, Ann Arbor, and others across the U.S.
But its intent is clear: Make sure the intangibles of principle are tucked into the algorithmic, and ensuing real-world decisions, that will shape the future of digital health.
Enjoy the rest of your weekend, readers. And seriously, please feel free to leave a comment with your thoughts right down below.



